PI3K/mTOR inhibition induces tumour microenvironment remodelling and sensitises pS6high uterine leiomyosarcoma to PD-1 blockade
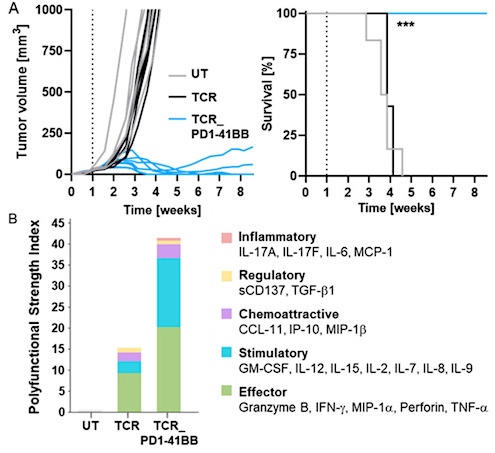
Abstract Abstract Background: Uterine leiomyosarcomas (uLMS) are aggressive tumours with poor prognosis and limited treatment options. Although immune checkpoint blockade (ICB) has proven effective… Read More »PI3K/mTOR inhibition induces tumour microenvironment remodelling and sensitises pS6high uterine leiomyosarcoma to PD-1 blockade