- Blog
13/01/2026


Novel immuno-oncology treatments show great promise in treating cancers. But with approximately 95% of oncological drugs that have shown efficacy in preclinical studies failing once they reach clinical trials, developing new treatments is no simple feat. To improve the likelihood of your immuno-oncology treatment gaining approval, selecting the right preclinical model is key.
It’s clear there is a significant barrier between preclinical studies and in-human trials, with many preclinical models lacking human relevancy to the system under study. In particular, advanced treatments work to target or harness the human immune system to combat cancer, infection, or inflammation — an aspect that traditional models struggle to recapitulate.
So, how do you choose the right preclinical mouse model for your immuno-oncology studies? In this blog, we explore four considerations that can help you choose the mouse model that accelerates the development of novel, safe, and effective oncology treatments.
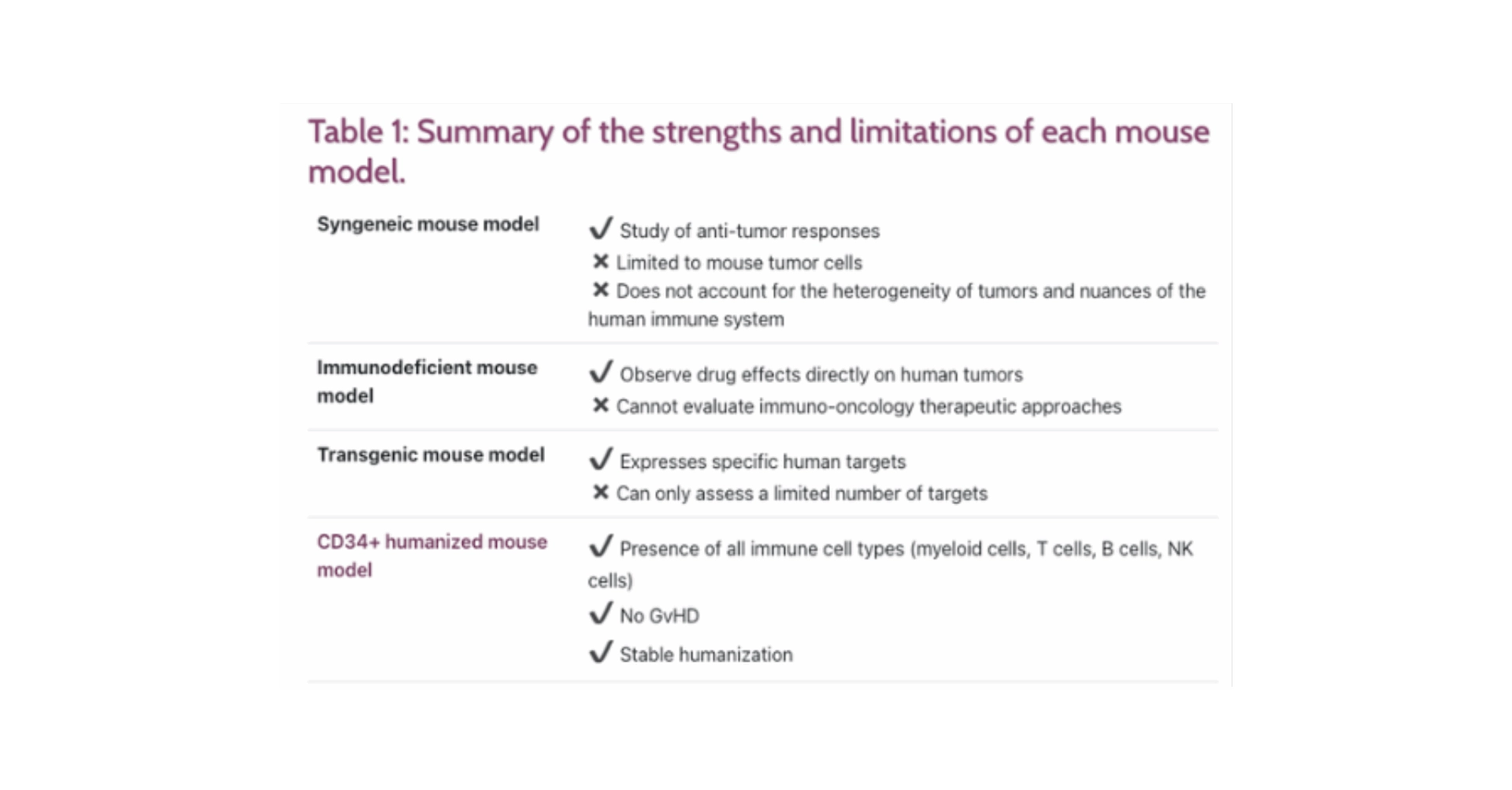
Not all mouse models are created equal. Several mouse models can be used for preclinical studies — namely syngeneic, immunodeficient, transgenic, and CD34+ humanized mouse models. Each model has its own strengths and limitations, as summarized in Table 1.
For immuno-oncology studies, humanized mouse models are the most representative model available, as they offer the deepest understanding of the human immune system. CD34+ humanized mice reconstitute all human immune targets, allowing them to accurately predict clinical immune response triggers.
A pivotal factor that complicates the choice of mouse model is the mechanism of action under investigation. Specifically, as immuno-oncological treatments recruit the immune system, the mouse model must be able to account for human-relevant interactions between the immune system and the disease for true insight into treatment efficacy and safety.
Take immune checkpoint inhibitors (ICPs), for example. ICP immunotherapy drugs block checkpoint proteins made up of immune cells, such as T cells, that stop the immune system attacking cancer cells. In these types of treatment, a mouse model such as the CD34+ humanized mouse model should be considered, as they can facilitate studies of both efficacy and mechanism of action in a single experiment.
Once you have decided on the most appropriate model for your studies, you should also consider variations within the mouse model. Mouse models vary significantly in quality, and three factors need to be taken into account when choosing your mice:
1- The cell source: Mouse models generated with donor blood, such as peripheral blood mononuclear cell (PBMC) mice, have differentiated lymphocytes, monocytes, and dendritic cells. However, these mice often show poor development of other immune populations. Cord blood can also be used, which is rich in CD34+ cells and offers superior engraftment properties.
2- The cell quality: High purity cells are essential. With CD34+ cells, for example, any CD4 or CD8 cell contamination can introduce GvHD, which both lowers animal welfare and can affect your results.
3- The mouse strain: A host of different immunodeficient mouse strains are available, but many lack the human cytokines needed to develop the human innate immune system. Look for a mouse model that can express human cytokines, to avoid any shortcomings.
4- Where to source your mice
After you’ve selected the ideal mouse for your immuno-oncology studies, the final puzzle piece is where to source your mice from. There are two main options available: a supplier and a partner.
A supplier will provide just the mouse and no additional services. This can be a cost-effective way to obtain your mice, given you have the necessary knowledge and equipment to perform the studies yourself. Many researchers, though, can be left feeling unsupported if they do not have the in-house expertise to perform the studies (particularly with models such as humanized mice), or require assistance with data interpretation.
A partner can support you throughout your studies, from initial discussions to experiment execution and data analysis. For those who are unsure which model is most appropriate, require access to cutting-edge technologies, or need assistance from specialists, working with a partner can be the best choice to maximize the potential of your studies.
Selecting the right mouse model for your preclinical immuno-oncology research is one of the most important steps you can take to increase the chance of successful outcomes in subsequent clinical trials. CD34+ humanized mouse models can fully recapitulate the human immune system, enabling you to get the deepest insights from your studies for more informed decision-making. By carefully considering your study needs, the mouse strain, and where you source your mouse model, you can unlock the true value of your experiments to develop safe and effective treatments more quickly.